Linda V. figured that if she could explain the dense, technical details of pharmaceutical manufacturing to industry analysts, she should be able to explain why she couldn’t sit through dinner. But after twenty years, she still struggles to get her point across.
Although she’s comfortable using the logical, impersonal communication style favored by engineers, that style can’t properly convey the emotional and physical impact of her sitting pain. And without understanding, it’s hard to secure the social grace necessary to function in a world designed for sitting.
Airplane Seats Are Supposed to Hurt, but Not like This
In 2001, Linda and her husband Dale flew to Italy, with plans to explore the country with their friends. Somewhere between Phoenix and London, Linda felt pain explode in the side of her butt and the top of her thighs. It was surprising, and horribly uncomfortable, but it got less intense once they arrived in Italy.
Rather than navigating a foreign health care system, Linda preferred to enjoy the time with her friends, so she did her best to ignore the pain. It spiked again on the flight home, and again, it faded after she got back to her house in Scottsdale, Arizona.
The following year, Linda and her husband flew to France. When they landed in Nice, Linda felt like she’d spent the trip sitting on a hot curling iron. This time, the burning pain stuck with her for the entire vacation.
Once again, the pain faded after she returned home, and Linda chalked it up to a quirk of her body. No one claimed air travel was comfortable.
But in 2006, the pain began to creep back in, and could be triggered by any activity that involved prolonged sitting. When she sat down to work, or went out to a restaurant, or settled in for a drive, she was distracted by the awful, burning pain in her thighs.
It was enough of a nuisance that Linda added the elimination of pain to her list of goals. She got regular massages, in case the pain was a consequence of tight muscles. When that didn’t work, she figured a well-designed exercise program would address any fitness shortcomings. She hired a personal trainer, and started swimming, hiking, and working out. Her overall fitness improved, but her pain did not.
On the Monday after Thanksgiving in 2007, Linda returned to the office to play catch-up after the long weekend. She was sitting at her desk when, at mid-morning, a bolt of pain shot through her right leg. It was as though someone had jammed an electric wire down the back of her thigh, and flipped the switch. She jumped so far, she nearly fell out of her chair.
She took the rest of the day off to see a doctor. She expected to be back at work in a day or two, perhaps with a new prescription bottle or a follow-up appointment. She didn’t realize she would never return to full-time work.

Searching for a Diagnosis
Linda went through the standard battery of tests – x-rays, MRIs, CT scans – but they failed to reveal any notable pathologies. Her doctors were stumped. Based on her pain description, it seemed clear that her sciatic nerve was responsible. They would chalk it up to back pain, except that she had an unremarkable back.
Linda’s pain was on both sides, though her right side was worse, which pointed toward a spine problem. But she had no herniated disc, no stenosis, and no fractures. Medical interventions intended for back pain patients (such as Lyrica, gabapentin, and corticosteroid injections) had no effect.
She was forwarded to physical therapy, where the therapist also treated her for a back problem. But the therapeutic techniques – stretching, foam rolling, and using a TENS device – actually made her pain worse.
Over the next four years, Linda traipsed from specialist to specialist. She saw fourteen doctors, but none of them could solve the mystery of her sitting pain. She tried alternative therapies, and visited an acupuncturist, a chiropractor, a yoga therapist, and a cranial sacral therapist. But none of their interventions reduced her pain. She visited a pain management specialist, and a chronic pain psychiatrist, but they did little to make her pain more tolerable.
As her doctors tried to puzzle out her symptoms, Linda did her best to cope with a difficult set of restrictions. She stood through meals at restaurants, movies, and meetings with friends.

Surgery to Free the Sciatic Nerve
While she was bouncing through the medical system, Linda also started searching online forums, trying to find people with similar issues. Her pain might be mysterious, but surely it wasn’t unique.
In 2011, she found a clunky old Yahoo! Forum (now defunct) where patients reported similar pain. Most of them had endured the same frustrating search, but there were also a few who reported successful treatment. Through them, Linda got the name of a surgeon, Dr. Hal Martin, who accepted the sorts of nerve entrapment cases that other doctors dismissed.
Dr. Martin had published several papers on something he called deep gluteal syndrome, in which the sciatic nerve is trapped in the soft tissues of the hip. Normally, the sciatic nerve is able to slide back and forth when a person walks, sits, or bends. But sometimes the nerve becomes stuck in muscles or scar tissue. When a person flexes their hip (say, by sitting, or pulling a knee to their chest), the nerve is forced to stretch rather than slide, which causes pain.
After reading about it, and talking to other former patients, Linda decided Dr. Martin’s ideas had merit. She made arrangements to visit his offices in Oklahoma City.
When she met with him, Dr. Martin reached underneath her thigh, and put his hand squarely on the painful spot. “Does this hurt?” He asked.
“I looked at him like, ‘Oh my God, I’ve found nirvana!’” Linda said. After going through countless appointments in which doctors questioned, debated, and dismissed her pain, it was validating to finally find a doctor who understood. “He was the light at the end of the tunnel,” she added.
Dr. Martin ordered new imaging tests, and conducted a thorough examination. He twisted her legs into various postures, prodded her hips, and checked her range of motion. When Linda described her symptoms, he seemed to know precisely what she meant. To Linda’s surprise, he could replicate her pain exactly.
Dr. Martin agreed she was a candidate for surgery, and scheduled a date in December. Together, they decided on a fairly conservative surgery. Although both of Linda’s legs were affected, Dr. Martin would only operate on the right side (her bad side). The piriformis muscle and tendon were, to the extent possible, left undisturbed.
During the operation, Dr. Martin removed a portion of the bursa by Linda’s femur, which was enlarged, and pressed against the sciatic nerve in certain positions. He also found a few areas where her nerve was trapped in scar tissue that formed around the deep muscles in her gluteal region. He extracted her sciatic nerve from these structures.
Linda also had an anatomical variation in which part of the piriformis tendon passed through her sciatic nerve. Dr. Martin freed the nerve from this interloper.
Once she had healed, Linda determined the surgery was moderately successful. It eliminated the pain in the middle of her glute, and she no longer felt like her leg was made of wood. But when she sat down, she still felt a burning pain in her upper thigh and lower glute. Since her left side hadn’t been touched, the pain there was unchanged.

The Pain Which Cannot Be Named
Dr. Martin’s tests helped pinpoint the source of her pain, and the surgery brought more relief than anything else she’d tried. Linda wasn’t completely cured, but at least she finally had a working explanation for her pain.
The anatomic variation that caused part of the piriformis tendon to pass through the nerve was congenital, and could not be prevented. But it, and other areas of nerve entrapment, were probably exacerbated by regular and extended periods of sitting. In Linda’s case, heredity and lifestyle combined to cause an unusual sort of pain.
Unfortunately, it was difficult to communicate her situation to others. Her condition remained nameless, and fell into the cracks between two murky diagnoses. Piriformis syndrome (a diagnosis which has many skeptics in the medical community) means that the piriformis muscle impinges on the sciatic nerve and causes pain. But other tissues were involved in Linda’s nerve entrapment, so the label of “piriformis syndrome” didn’t fit her properly.
Deep gluteal syndrome was a catch-all diagnosis, and a largely unrecognized one. Since Linda’s condition included aspects of piriformis syndrome, deep gluteal syndrome wasn’t the right label either. She preferred to use the accurate, though less precise, term “nerve entrapment” to explain her condition.
During her freelancing phase in the late 90s, Linda worked with many unknown software startups, and managed to get each of them ranked among the top 5 in their category. Her PR skills were not in question. She was confident she could use the same techniques to build awareness of her unique ailment. And so, she set about writing executive summaries, submitting guest blog posts, and talking about her situation on a local radio program. She personally explained her condition, again and again, to friends and family members.
But she hit a wall of confusion that no amount of explanation could overcome. Although she’s been living with nerve pain for nearly twenty years, well-meaning friends and family still ask, “How’s your back?”
“It’s as if I had a broken arm for twenty years, and people ask, ‘How’s your nose?’” Linda said. “I have a master’s in communications, and I’m not getting through to people.”
Recently, she had a long conversation about her condition with a family member. Afterwards, he and his wife sent Linda two books: one about an alternative therapy called tapping, and one by John Sarno that blamed back pain (back pain!) on internalized emotions. Their intentions were good, but these gifts revealed a fundamental lack of awareness.
But educating her friends and family was nothing compared to convincing bureaucracies – such as her insurance company – that her condition was real. Her diagnosis doesn’t have a proper name, let alone a medical code, and doesn’t fit neatly into an established organization system for pathologies.
When it became clear that she couldn’t return to work, Linda filed a disability claim. This led to an extended back-and-forth, in which Linda submitted records of her income loss and medical assessments. She met with a vocational consultant, who tried to find a suitable alternative to PR work, but couldn’t think of any feasible ideas. Still, the insurance company denied her claim. Later, the Social Security Administration denied her application for disability benefits.

To Make Matters Worse: Other Health Complications
Her sitting pain made work enough of a challenge, but Linda also developed unrelated health problems that further limited her options. In 2004, she started noticing pain in her hands. Her mother had the same problem, and like her mother, Linda got progressively worse. Doctors diagnosed her with both tendonitis and arthritis, but there wasn’t much they could do.
PR work mostly involved sitting and typing, so this was a serious impairment. Linda slowly lost the ability to type, or do any task that required a firm grip or fine motor control. She purchased state-of-the-art voice recognition software to help with transcription, but it was buggy, and couldn’t help with many computer-related tasks.
After seven years of standing while others sat, the veins in her legs gave out. One day, Linda was outside walking when she felt a sudden, intense burning in her legs. Although she could barely walk, she didn’t have a choice. She had to get home somehow.
Once back, she convinced her husband to take her to a doctor, who traced the source of the pain to multiple collapsed veins, which a vascular surgeon burned away. That solved the immediate problem, but didn’t address the underlying cause: venous reflux.
In this condition – which Linda’s mother also had – the valves in the veins stop functioning properly. Although Linda’s only symptom was pain, venous reflex can cause a host of other vascular problems, including swollen legs, varicose veins, and cramps.
Over the next three years, Linda had regular vein problems each summer, and underwent several vein ablations. But she only had so many veins in her legs, and the vascular surgeon eventually advised against destroying any more.
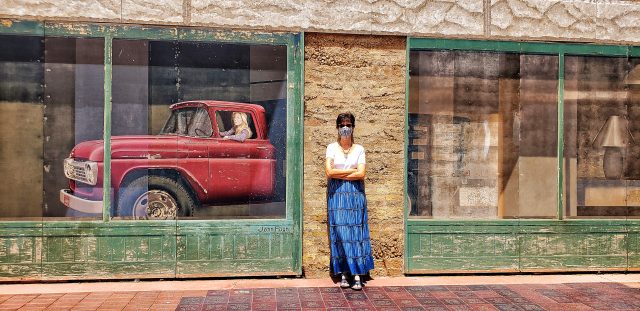
These days, Linda manages her venous reflux by wearing compression hose and limiting her standing time. “In the summer, I wear skirts,” Linda said. “Which isn’t a normal outfit for me. But knee-high hose with capris is not a good look.”
Genetics is a risk factor for venous reflux. So is being a woman. A third is standing too much. “But since I can’t sit, what am I going to do?” Linda said. “When people talk about standing desks, that’s an aspect that doesn’t get mentioned.”

Free Business Idea: Sew an ice pack sleeve into the seat of a folding chair. Collect money.
Does Anybody Want Me?
If her health crises hadn’t forced her to retire, Linda would have kept working in PR until the day she died. She specialized in public relations for process manufacturing, which involved deeply technical discussions with engineers, industry analysts, and startup founders. When she wasn’t busy touring pulp mills, power plants, and pharmaceutical manufacturing centers, she was churning out white papers and press releases, and lugging press kits around on far-flung press tours.
She loved advocating for her clients, hobnobbing with industry leaders, and being the first to know about major technical leaps. Her frequent business trips took her to exotic locales, and she met hundreds of smart and talented people.
“That was my whole identity,” Linda stressed. “I just loved interacting with other people in tech. I was really, really excited and happy.”
When it was clear she couldn’t go back to her old job, she was crushed. But she was also determined to do something meaningful with her time, so she started looking for other career paths. She considered teaching college courses, and got her teaching certification, but then realized she needed an advanced degree to get hired.
She started a book blog. That hobby taught her how to run a website, and gave her an excuse to interview authors. She worked on a family genealogy, labelled everything at home, and volunteered as a speaker to educate groups about hospice care. When her mom got cancer, Linda started making regular trips to Rhode Island to assist her mom and help get her affairs in order.
She changed the focus of her self-owned business in 2016. Instead of doing PR consulting, she started analyzing the business plans of new entrepreneurs. But since she couldn’t sit without pain and couldn’t type, she struggled to keep up with the physical demands of the work. Besides, she learned that few entrepreneurs wanted to share their business plans. After two years, she dissolved the business.
She looked into becoming an antique auctioneer, but found out most of the work happened online. She applied to work in an assisted living facility, but they decided she wasn’t qualified.
“I started to think, does anybody want me?!” Linda said. “How do you find meaning in life when so many options are limited?”

I’m Like a Hummingbird
“Now that I’m 61, it’s more acceptable to not be working,” Linda explains. Her husband recently retired from his job in IT sales as well, so the two of them can spend more time together. They divide their time between Scottsdale and Flagstaff, Arizona, where they enjoy the reliably warm weather and scenic walks.
Like many people with chronic pain, Linda has learned how to budget her time and energy. “Every day is scheduled around the times when I absolutely have to sit,” Linda explained. “The rest of the time, I’m moving, cleaning, walking, talking to people. I’m like a hummingbird – I keep flitting from place to place.”
She tolerates sitting on soft surfaces better than hard surfaces. When she needs to sit, she stacks cushions on her seat, or uses a folding chair designed to take the pressure off her thighs. Ice packs also help control the pain, and she travels with a cooler full of them.
“Pre-COVID, if I showed up at a friend’s house, they’d all laugh,” Linda recalled. “It would take me two trips from the car to bring everything. I used to be self-conscious. I got over that.”
When she gets together with friends, it’s usually for breakfast. Her pain tolerance is highest first thing in the morning, and breakfasts rarely become drawn-out affairs.
Though she tries to take care of herself and manage the sources of her pain, sometimes she crosses the threshold without realizing it. “It’s like an electric dog fence,” she said. “You don’t always know you’ve crossed the line until it’s too late.
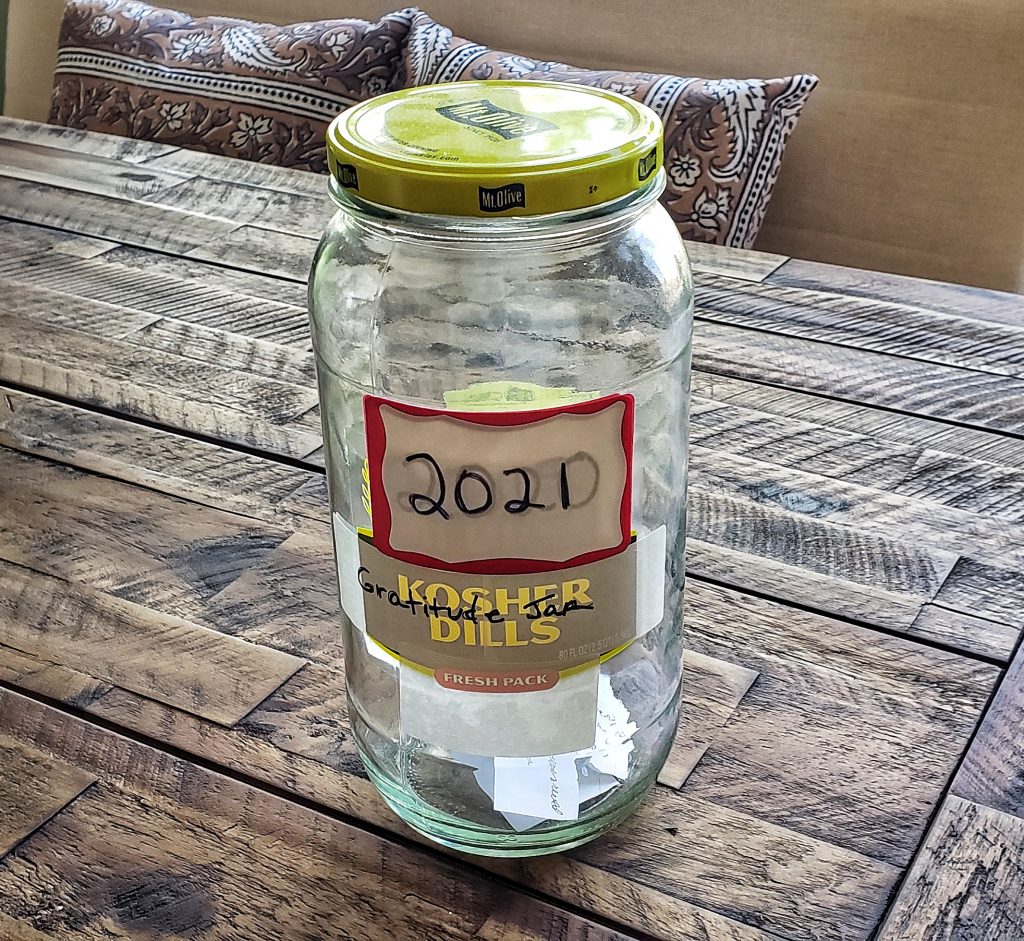
She’s also found ways to cope with the mental and emotional stress of living with chronic pain. In 2013, she started a gratitude jar. Whenever she notices some small blessing, she writes it down on a slip of paper, and puts the paper in the jar. On New Year’s Eve, she empties the jar, and reads the record of beautiful moments. She recalls beautiful days, acts of kindness, and sugary treats from Dunkin’ Donuts. Some years, the jar is more full than others, but she inevitably finds good memories that she forgot about.
A PR Campaign for Sitting Disabilities
Linda has not completely given up her PR campaign. When her health allows it, she promotes awareness of sitting disabilities, and reaches out to experts who can help overcome the myriad obstacles that people with sitting disabilities face.
These obstacles include design challenges; public spaces, cars, restaurants, and even houses are designed to accommodate sitting. They also include a lack of recognition by medical and insurance companies, and oversights in the ADA and other legislation.
She’s also learned to be her own advocate. “We’ve always revered medical specialists, but you have to take your health into your own hands,” she noted. She takes notes during medical appointments, and asks doctors to share their clinical notes afterwards.
“A lot of times, you read their summary, and think, that’s not exactly what we talked about,” she explained. “If you have to submit things to social security, or insurance, you want an accurate representation of what happened.”
She’s also learned to treat herself kindly. In the beginning, she tried to force herself through painful experiences in order to keep up the appearance of normalcy. But the act was fatiguing, and she couldn’t keep it up indefinitely. Better to be honest about her limitations, and work within her capabilities. That way, she could reserve her limited resilience for the things that mattered.
You are amazing person Linda. I am Blessed to know you and have you as a summer neighbor. Hope you can make a few trips this winter also. You always have a smile. I have learned through difficult times in my life and the years my husband was in pain I think we can be happy even we are sad because we have so much to be thankful for the beauty of the snow fall and how peaceful’ sun rise no and all the beautiful things you and Dale see on your walks. Thank you for sharing your struggle you are a strong and beautiful person. I am great full to have you both in my life
Kudos to Krista for such an accurate rendition of my condition, and thanks to Rose for your wonderful comment.
Very clear and informative article. The insurance companies and the SSA should provide service, not obstacles to the people they are’s supposed to help.
A great representation of your pain here, it can be so difficult to explain chronic pain to people.
Mine is similar, but sitting or laying down relieves it, though we both know comparisons should never be considered. We are all individuals.
I found it interesting to read of the different treatments tried. You have been through a lot in the medical community. I felt the disappointment of losing job, purpose, self, etc throughout discovery of limitations. Depression can easily take over, but you have powered through trying to find new meaning. That takes strong mental calculation and strength.
Also, chairs with ice packs and no hard edges would be amazing inventions.
Your gratefulness and camera and visions you share are appreciated very much, I’m glad you can still find ways to be joyful and enjoy moments of life despite pain. I know how hard this can be.
Thank you for sharing this article!
Fantastic rendition of your story and your pain experience. I’ve always known you were one of a kind, but your determination and strength take you into a category known by very few. I will forever respect your pain and your tolerance to overcome it. You are brave and beautiful and loved hearing your story of courage and power.
Thank you for sharing!