A disc herniation is a simple concept to explain. A bit of disc material crosses the border, and starts occupying space that belongs to other tissues.
But when I started reading up on disc herniations in an effort to understand my own, I realized that this simple definition belies the complex nature of the tissues and processes involved. The disc itself is an impressive feat of engineering, but it also has fatal weaknesses. And once structural integrity has failed, the disc is capable of wreaking havoc on the body to a degree inconsistent with its small size.
What a Disc Is Made of
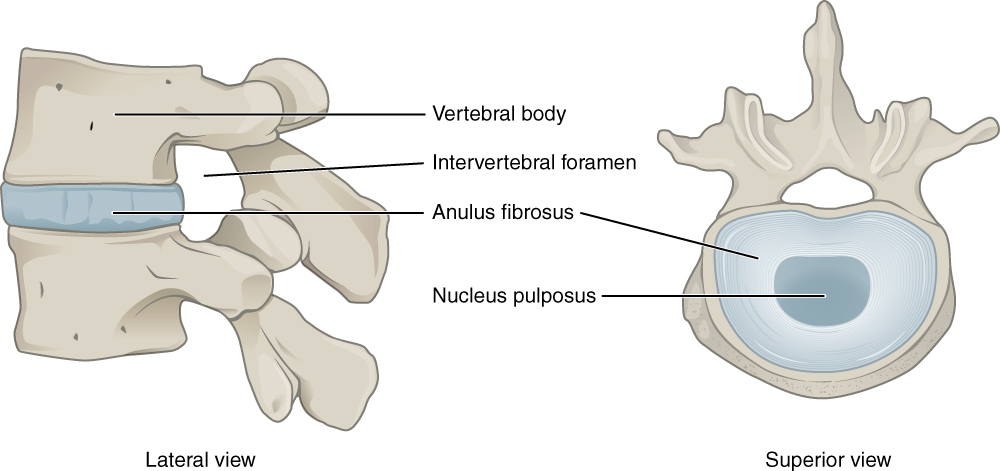
If you’ve talked to your doctor about a herniated disc, she probably explained that there are two different layers. The outside ring (called the annulus fibrosus, or just annulus) is tough and solidly attached to the vertebrae, while the center (called the nucleus pulposus, or just nucleus) is squishy and gelatinous. She may even have compared your disc to a jelly doughnut.
This is a decent analogy, although as I’ve written, a better dessert-themed analogy is a lava cake.
The annulus is made of type I collagen, which is the most common type of collagen in the body. It’s particularly good at absorbing tensile forces, meaning it can stretch and rebound without breaking. This property makes it an ideal building material for many of body’s tissues, including tendons, bones, and scar tissue. One textbook observed that gram for gram, type I collagen is stronger than steel.
These collagen fibers are arranged into about twenty concentric circles, which are connected to each other by elastic proteins. The makeup of the annulus follows a gradient from the exterior to the interior, as the types and quantities of molecules change. The annulus rings near the center of the disc start to resemble the nucleus.
The nucleus mainly uses type II collagen, which is also found in joint cartilage. Type II collagen molecules are thinner than type I molecules, and tend to form complex networks with other types of collagen and water-grabbing proteins. In this arrangement, type II collagen molecules provide strength, while the other collagens and proteins provide viscosity. The resulting matrix is particularly good at absorbing compressive forces.
The two types of collagen team up to handle common stresses. When compressive force is placed on the spine (say, because you picked up a heavy suitcase), the nucleus is placed under pressure, and redistributes the force equally around its perimeter. This places the type I collagen fibers in tension, as they bulge slightly outward.
In summary, the nucleus is great at absorbing and redistributing compressive forces, and the annulus is great at handling the resulting tension. It’s a marvelously effective system, as long as everything is going well.
Another interesting collagen fact, which has nothing to do with disc herniations, has to do with its role in scurvy.
You might be thinking, wait, but what about the lemons?
It turns out that vitamin C is required to convert molecular precursors into actual collagen. Bones, tendons, blood vessels, and skin all rely on collagen for structural support. Without it, they are easily damaged. This leads to the characteristic symptoms of scurvy, like diseased gums, easy bruising, and slow-healing wounds.
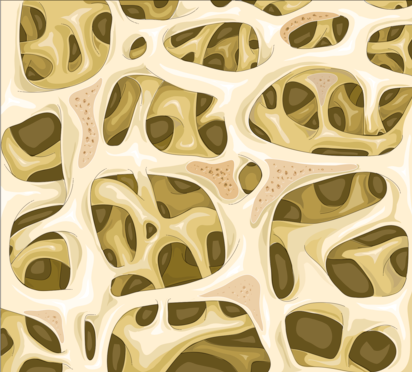
Breaking Bones
Each vertebrae has a thin, cartilaginous membrane called the end plate on its top and bottom. (Although some sources refer to the end plate as part of the disc.) The outside of the vertebrae is made of solid bone. Inside is a lightweight network of bone that looks very much like a sponge. This interior matrix can deform and spring back into place, although it often sustains tiny fractures in the process.
If a person is young and healthy, and the stress is moderate and occasional, then these tiny fractures are no big deal. The bony network will be repaired, and the vertebrae may become even stronger. But if the stresses are continuous (say, because your job involves loading and unloading trucks for hours) or if the bony network is already weak (say, because you have osteoporosis), then the vertebrae may be damaged beyond repair.
If the spine is subjected to a compressive force without bending (say, because you slipped on the ice and landed flat on your rear), the vertebrae will fail before the disc’s annulus does. When the spine is placed under compression, the disc’s nucleus doesn’t just bulge outward. It also bulges up and down into the vertebral end plates.
Depending on the force and speed of the load, either the end plate or the bony vertebrae will fail first. When the end plate fails, it cracks, which allows the gel-like material from the nucleus to seep into the vertebrae’s airy interior.
This will result in a loss of disc height (since some of the disc material moved out), and for this reason, imaging scans may be deceptive. Compressive vertebral injuries don’t show up well on X-rays, and doctors are likely to diagnose degenerative disc disease, or a herniated disc, even though the annulus is still intact. (Technically, this kind of injury can be classified as an intravertebral herniation.)
Breaking Through the Annulus
So if compression doesn’t cause the disc’s annulus to fail, what does?
Unlike bone, the collagen layers of the annulus are unlikely to break. Instead, they fail by delamination, meaning the individual fibers separate from each other.
If nuclear material has already been lost (say, as the result of an end plate fracture), then the disc stops behaving nicely under compression. Instead of bulging outward, part of the annulus collapses inward, which encourages the layers of the annulus to separate.
Bending is also tough on the disc. It causes the collagen fibers on one side of the annulus to be compressed, while fibers on the other side are stretched. The nucleus also directs all forces to one side during a bend. If the layers of the annulus have already started to separate, the nucleus will seep into the gaps.
The delamination that leads to a disc herniation happens from the inside out. As layer after layer of the annulus is pulled apart, the nucleus pushes through, until it breaks out of the disc entirely.
If you want to make darn sure a disc will herniate, the best way to do it is by bending forward as far as you can while holding something heavy. The combination of full flexion and compression is guaranteed to destroy your spine.
Invasion
A healthy disc is an inhospitable place. Only a few hearty cells (which make up less than 1% of the disc’s volume) can survive in the interior, which is notably lacking in both blood and oxygen.
Delicate structures like blood vessels and nerves can only penetrate a couple of millimeters into the annulus. Inside, the compressive forces are so high that they would obliterate these fragile tissues. The cells inside the disc rely on nutrients that are passed through the end plates.
However, damaged discs are unable to sustain such high pressure, and blood vessels and nerves start to invade. The new blood vessels feed colonies of new cells, which may be an attempt by the body to repair itself. These blood vessels also stimulate nerve growth, and it’s thought that these new nerves might partially explain the pain reported with disc degeneration. However, this is still more idea than explanation.
Interestingly, experiments done on pigs, dogs, rabbits, and rats indicate that nuclear material is uniquely damaging to nerves. The applications for humans aren’t well understood, though. Researchers can’t run the same types of experiments (such as surgically cutting a gash in the annulus) on humans.
Classifying Herniated Discs
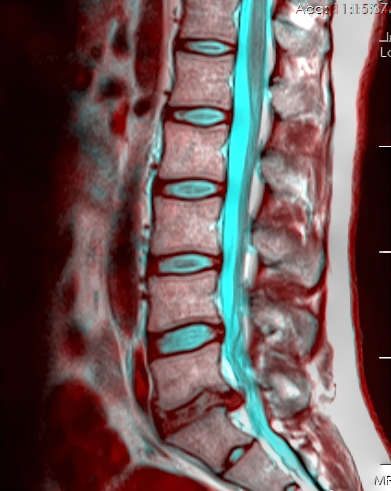
When I was running my first lap of medical exams (x-rays, EMGs, MRIs, and blood tests), I remember being confused by some of the terminology I read in my radiology reports. My MRI report noted that I had a “concentric disc bulge,” and a “paracentral disk extrusion” at the L5-S1 level, and a “concentric disk bulge” and “paracentral disk protrusion” at L4-L5.
But what was the difference between a bulge, an extrusion, and a protrusion? Was the radiologist just showing off?
Apparently even experts got annoyed at the jumble of jargon, so in 2001, several professional organizations (including the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology) teamed up and authorized a task force to sort out the semantic mess.
Their recommendations, which have been widely adopted, tried to limit the use of overlapping terms and properly define the remaining terms.
Annular Tear/Annular Fissure: The task force got off to a rocky start, since these two terms mean the same thing. They’re actually fairly broad, and mean the annulus is messed up. They could mean that several layers of the annulus have separated, that annulus fibers were pulled away from the vertebrae, or nearby fibers have pulled apart. The presence of an annular tear does not necessarily mean the disc is herniated.
Herniation: This is the term used when part of the disc has escaped beyond its borders. Although the nucleus often pushes through its annular border, a herniation is also possible when bits of the annulus or other tissues escape.
Intravertebral Herniation: As mentioned above, compressive forces can cause the vertebral end plates to fracture, and disc material can seep into the bone. This is called an intravertebral herniation.
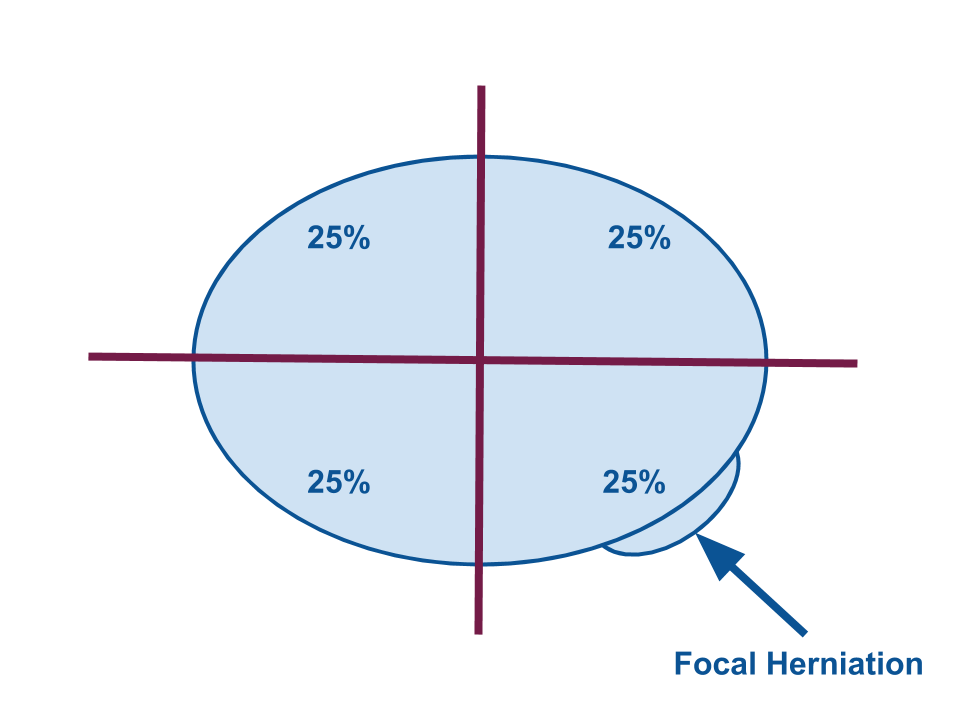
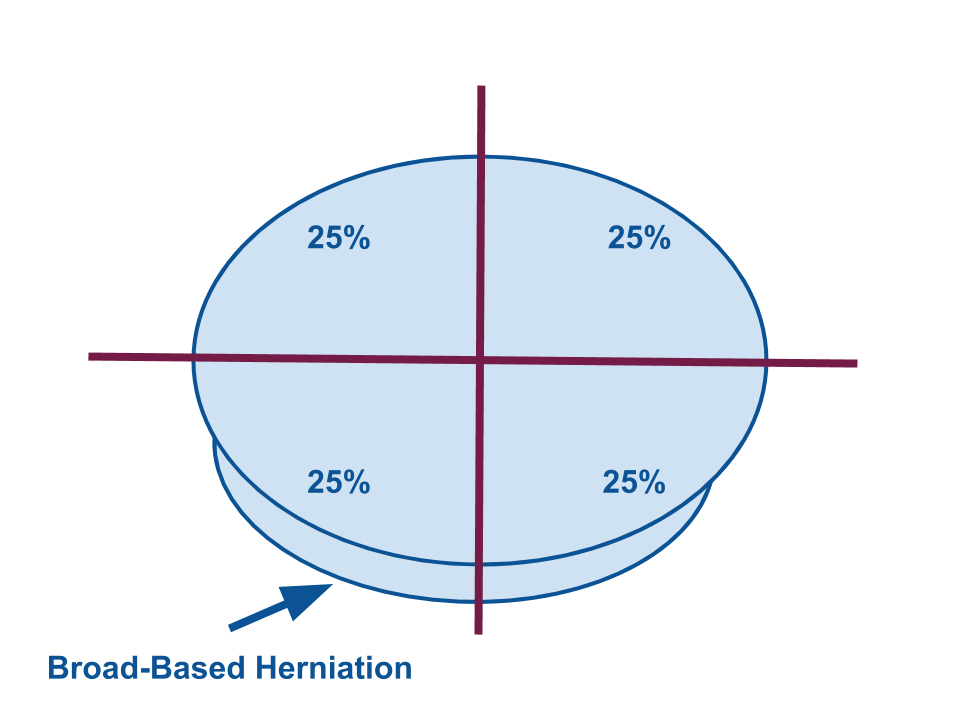
Focal and Broad-Based: These are mutually exclusive categories. In a focal herniation, the base is less than 25% of the disc’s circumference. In a broad-based herniation, the base is between 25-50% of the circumference. This is much easier to understand with a picture.
Bulging: A disc bulge is not considered a type of herniation. The term is used when the base of the would-be herniation accounts for more than 50% of the disc’s perimeter.
Contained and Uncontained: If the annulus is still acting as a barricade between the herniated material and the tissues outside the disc, the herniation is contained. If the annulus has been breached, the herniation is uncontained.
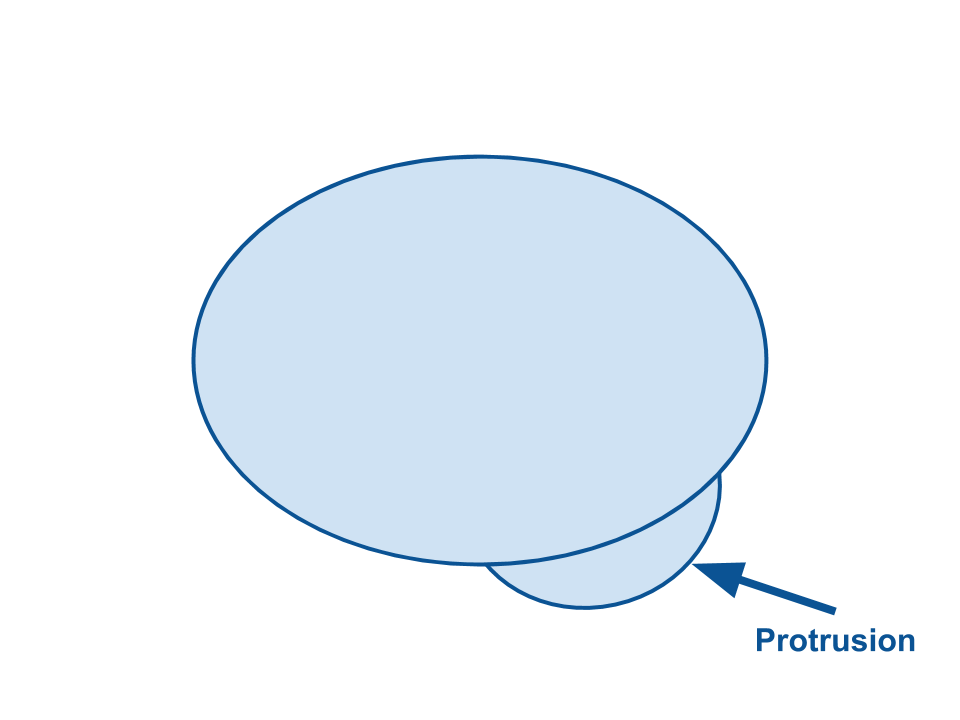
Protrusion and Extrusion: A herniated disc is either said to have a protrusion or an extrusion. The categories assess shape. A protrusion will have a wide base relative to the shape outside the disc. On scans, it will look like a hill. An extrusion will have a comparatively narrow base, and will look more like a mushroom.
These terms are also difficult to puzzle out without pictures, so, here:
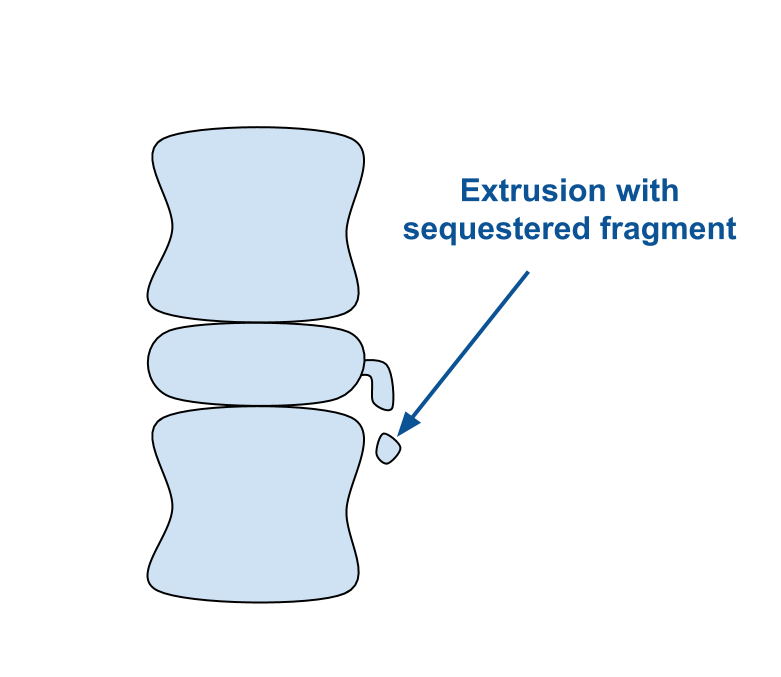
Migration: If the extruded material from the disc starts to poke around in another direction, it’s said to have migrated.
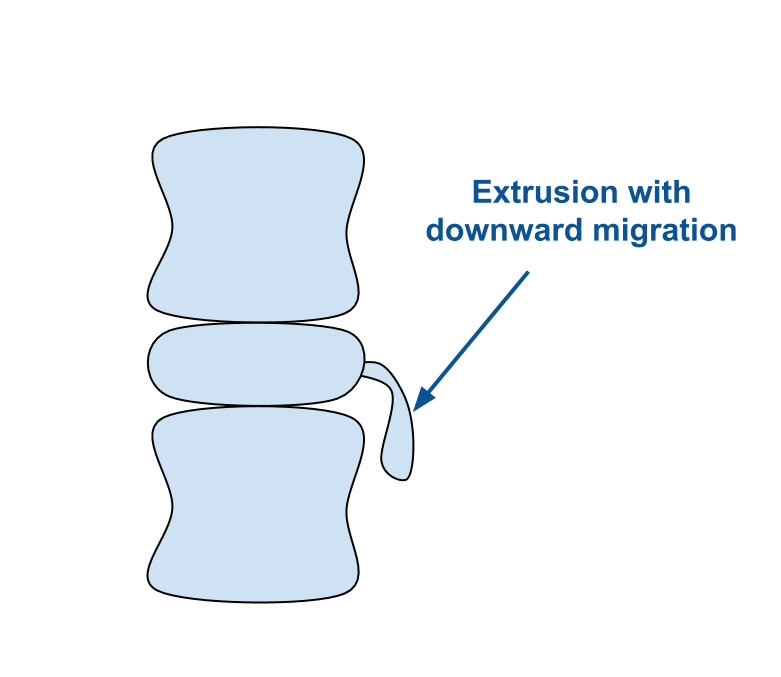
Sequestration: If a piece of the extruded material breaks off so that it’s floating freely outside the disc, it’s said to be sequestered.
Sources
- Low Back Disorders, by McGill S. Human Kinetics, Inc.; 2015
- Molecular Cell Biology, 4th ed., by Harvey Lodish, Arnold Berk, S Lawrence Zipursky, Paul Matsudaira, David Baltimore, and James Darnell. W. H. Freeman; 2000.
- “Nomenclature and Classification of Lumbar Disc Pathology,” by David F. Fardon, MD, and Pierre C. Milette, MD. SPINE Volume 26, Number 5, pp E93–E113. 2001.
- Rothman-Simeone The Spine 7th Edition, by Bell GR, Garfin SR, Fischgrund J, Eismont FJ, Bono CM. Elsevier; 2017.


3 thoughts on “Disc Herniations: A Failure Between the Bones”