Before I got my first epidural injection, my doctor confidently predicted that they would wipe out my sciatica…Eleven shots later, I was seriously questioning whether these shots were capable of curing anyone.
Exactly three years exactly after that first injection, I was excited to see a brand-new, published-ahead-of-print paper that tried to parse out what effect epidural injections had on sciatica. The Cochrane review was entitled, Epidural corticosteroid injections for sciatica.
One frustrating barrier to evaluating sciatica treatments is the tendency for researchers to lump sciatica in with other types of back pain. While I understand the connection, the conflation makes it difficult to tease out any differences that might exist. This review, however, focused specifically on sciatica.
About the Study
This was a review paper, which meant the authors didn’t conduct any new research studies. Instead, they looked at studies that had already been published, reanalyzed the data, and compared results from multiple studies in order to draw larger conclusions.
An earlier incarnation of this study was published in 2012 in the Annals of Internal Medicine. In both cases, the authors carefully evaluated the quality of the data, and rated it based on potential biases. Data could be downgraded because of factors like flawed study design, inconsistent results, or small sample size.
Before the authors could really get started, they needed to decide which studies to include in their review. They narrowed their search to include only randomized trials that compared epidural injections to a placebo. The final paper includes data from 25 clinical trials.
They also divided studies into sub-groups to determine whether certain factors would affect the outcome. They focused on:
- The method used to administer the injection
- Whether or not fluoroscopic guidance was used
- Which type of placebo was used
- How the diagnosis of “sciatica” was determined
You don’t have to remember these factors, because – Spoiler! – none of them were shown to impact the final results.
It’s also worth knowing which factors were left out. There are a lot of variables which might impact results, and researchers don’t have the time or resources to analyze every possibility, so some elements fall by the wayside.
Factors that were not considered include:
- The underlying cause of a patient’s sciatica
- The type of corticosteroid used
- The specific dose
- Effectiveness of multiple injections vs. single injections
The main outcomes the authors concerned themselves with were leg pain intensity and disability. Both were determined using patients’ self-reported responses to questionnaires.
Secondary outcomes included back pain intensity and overall pain intensity, which were also determined using patients’ self-reported responses. They also tracked adverse events (which are basically bad side effects).
For all outcomes save adverse events, the researchers converted study results to fit a 0–100 point scale, where 0 = no pain/disability, and 100 = worst possible pain/disability. This conversion allowed researchers to properly compare the results of various studies.
So, Did Epidural Injections Help?
A little bit, but only in the short term.
Before I go any further, let me add a caveat. Based on the data evaluation mentioned above, the researchers rated the quality of evidence used to draw various conclusions between moderate and very low. (Evidence is sorted into four tiers – High, Moderate, Low, and Very Low.) This is the authors’ way of saying they reserve the right to change their minds if they’re presented with new and better data.
Leg Pain
Compared to placebo, epidural injections did reduce leg pain immediately afterwards (within 2 weeks of the injection). However, the difference only amounted to 15 points on a 100-point scale.
In the short term (2 weeks – 3 months), leg pain was reduced by about 5 points.
Only one study recorded leg pain in the intermediate term (3–12 months afterwards), and it showed a slight increase in pain scores (9.1 points) for those receiving an injection.
The three studies that reported long-term (more than 12 months) leg pain reported no difference between injection and placebo.
Disability
The results for disability were even more tepid. The differences between placebo and injection for all time periods were practically nonexistent, although it’s worth noting that the quality of evidence was slightly lower than for leg pain.
Back Pain
As with leg pain, the differences were most notable in the immediate (-10.8 points) and short (-2.0 points) term. The intermediate and long-term results showed that those receiving an injection had slightly higher pain scores, though my non-expert reading is that the differences could be due to statistical weirdness.
Overall Pain
Those receiving injections had slightly lower pain levels in the immediate (-4.7 points), short (-9.4 points), and intermediate (-4.9 points) time frames. The long-term pain levels were reported as slightly higher (6.9 points) for those who received injections.
What Adverse Events Were Reported with Epidural Injections?
In most of the included studies, adverse events were something of an afterthought. Studies differed in how closely they tracked adverse events, and reported them in different ways. The authors noted that, “[O]nly one third of the included studies appropriately reported the occurrence of adverse events separately for the treatment and placebo group.”
The reporting of adverse events seems awfully idiosyncratic, so I’m hesitant to draw any firm conclusions based on the reports in this review. Still, I’ll include a list to give you a sense of which complications can occur.
Adverse events included:
- Non-specific headache
- Dural puncture
- Worse pain/leg pain
- Localized pain
- Nausea
- Tinnitus
- Irregular periods in women
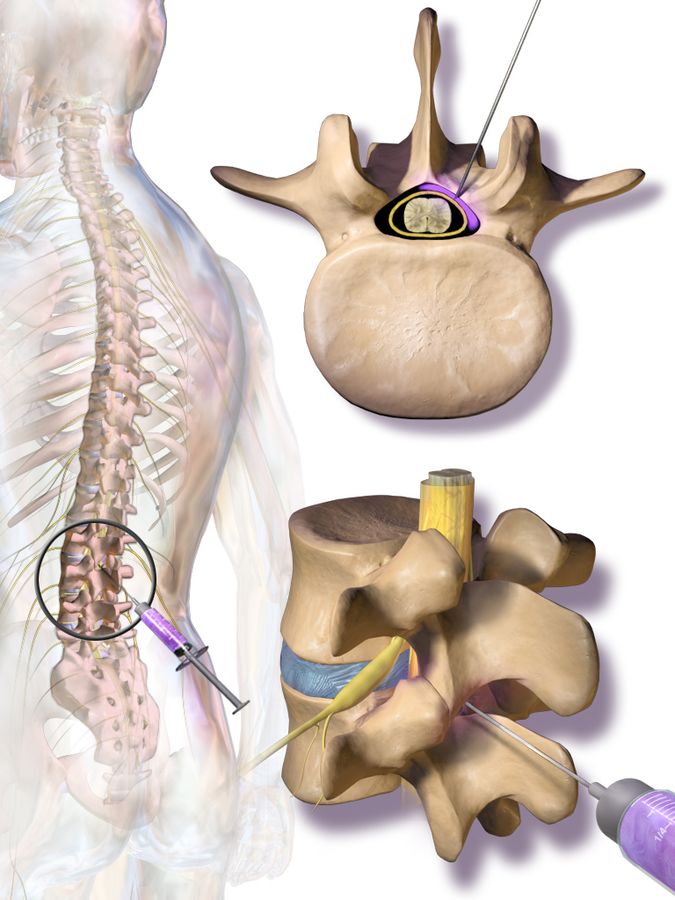
“Dural puncture” refers to an incident where the needle penetrates the dura mater (a sheath around the brain and spinal cord). It can cause severe headaches, nausea, vomiting, hearing loss, tinnitus, dizziness, and other unpleasant symptoms. Several of the reported events overlap with side effects of dural puncture, though it’s not clear whether they’re due to dural puncture, a bad reaction to the medication, or some other cause.
Which Is Worse? Sciatica, or Low Back Pain?
Warning! Tangent alert!
I found it oddly validating to read that, “In comparison with patients with low back pain alone, patients with sciatica usually report higher disability and pain intensity as well as higher rates of work absence.” I’ve experienced both, and I can say with absolute confidence that sciatica is to back pain what evisceration is to a bellyache.
My back-pain experiences tend towards the comedic. One incident in particular led me to spend an afternoon traipsing around Brooklyn, in search of an open clinic, and then a well-stocked pharmacy.
I went to bed with a stomach full of over-the-counter painkillers, and woke up feeling like my head was both floating in the clouds and underwater. There was a ringing in my ears, and my body had lost interest in obeying my brain’s commands. That was how I learned that it is possible to overdose on aspirin.
My sciatica, however, runs tragic. It led to unrelenting torture, disability, desperation, and despair. Once, I stayed up (literally standing on my feet) all night because of unrelenting cramps. The next morning, I tried to go to work anyway, but the pain only intensified until I went home sick.
After consulting with two doctors and my insurance’s Dial-A-Nurse program, I went to the emergency room, where the doctors dismissed my symptoms, gave me a prescription for naproxen, and sent me home. It took me about fifteen minutes to get into the car because my legs were too spastic to bend voluntarily.
I cried uncontrollably. I didn’t laugh.
Worth a Shot?
Listen, I’ve had my share of terrible days and nights. There were times when I would have traded a limb to get rid of my sciatica. Epidural injections seemed like a no-brainer, and I would never judge anybody who signed up for them.
But the results of this paper suggest patients should set their expectations appropriately. If you’re looking for temporary pain reduction, epidural injections may help. Of course, there’s also a small but real chance that you’ll end up with a serious headache, or other unpleasant side effects.
But there is no evidence to show that epidural injections will cure you, or do much of anything in the long term.
You might also like:

2 thoughts on “New Study Asks, “How Well Do Epidural Injections Treat Sciatica?””