In a fight between the vertebra and the disc, which would win?
The answer, surprisingly enough, is the disc.
Scientists have known since 1927 that the nucleus pulposus is quite capable of punching through the vertebrae’s endplate, rather than escaping through a fissure in the annulus. This sort of damage can lead to a wrinkly puncture mark, known as a Schmorl’s node.
At first, it seemed like mechanical damage was all there was to the story. However, once the role of genetics in back pain was becoming understood, scientists decided to investigate whether Schmorl’s nodes might also be heritable.
This article explains what Schmorl’s nodes are, how they come about, and what role genetics play.
What are Schmorl’s Nodes, and What Causes Them?
A Schmorl’s node is a defect on the vertebral endplate, which results from a type of disc herniation in which the nucleus pulposus punches through the cartilaginous endplate and pushes into the bone.
It used to be thought that the intervertebral discs were the shock-absorbers of the spine. However, there is now good evidence to suggest that the vertebrae themselves serve this function.
The disc’s nucleus is non-compressible, so if the spine is compressed while in a neutral position (say, because the person is carrying a couch), the nucleus will cause the endplate to bulge into the body of the disc.1
If the compressive force (which can be due to either a one-time event, or repetitive loading) is great enough, it’s the vertebra that will fail first. The endplates will rupture, and nuclear material will seep through the cracks.5
In Low Back Disorders, Dr. Stuart McGill notes that, “Over the years we have compressed over 400 spinal units in a neutral posture, and all but 2 resulted in end-plate fractures as the primary tissue damage.”4
Even relatively small loads (20–30% of a one-time failure load) can cause microdamage that will lead to failure if repeated often enough.4
Some researchers believe that physical activity in young adults can also lead to Schmorl’s nodes, even if they don’t lift enough weight, or lift it as often, as an adult would need to in order to cause a similar injury.2
The thinking goes something like this: The epiphyseal plates in the vertebrae don’t fully fuse until a person is in their mid-20s. Before that time, the fibers of the annulus attach to the unfused epiphyseal plates. Twisting can weaken the endplate and cause microfractures, which gradually expand, and form Schmorl’s nodes.
For reasons that are not completely understood, Schmorl’s nodes tend to be concentrated in the lower thoracic and upper lumbar region (T7–L1), and are more likely to occur on the undersides of vertebrae than on the top sides.3
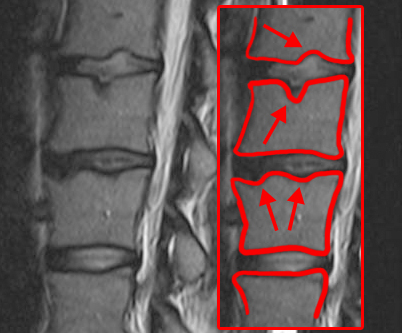
Photo courtesy of J. Lengerke via Wikimedia Commons.
Are Schmorl’s Nodes Painful?
The endplate damage that leads to Schmorl’s nodes doesn’t always cause pain – one study showed that 19% of patients without back pain had Schmorl’s nodes on imaging scans.3
In other cases, endplate damage leads to pain that is immediate and acute. Pain stemming from endplate damage is often misattributed to disc herniation or disc degeneration.
Here’s McGill again, explaining the difference:
“In my experience, end-plate fracture with the loss of nuclear fluids through the crack into the vertebral body (often forming Schmorl’s nodes) is a very common compressive injury and perhaps the most misdiagnosed. Loss of the disc nucleus results in a flattened interdiscal space that, when seen on planar X-rays, is usually diagnosed as a herniated disc or degenerated disc. However, the annulus of the disc remains intact. It’s simply a case of the nucleus squirting through the end-plate crack into the cancellous core of the vertebra…When compressing spines in the lab, we hear an audible pop at the instant of end-plate fracture—exactly what patients report when they describe details of the event that resulted in their pain…If there is substantial loss of the nucleus from the disc (i.e., it is vertically herniated), then immediate loss of disc height and subsequent compromise of the nerve root space will result. At this point the end-plate fracture will mimic the symptoms of true herniation–another reason for the common misdiagnosis.”4 (pg. 56)
People with endplate damage are often sensitive to compression, especially when the spine is in a neutral position. The heel-drop test is often a useful diagnostic tool. In contrast, people with typical disc herniations will find compression more painful when their spines are flexed forward.
Side note: If you’re interested in self-administered tests to help identify the source of your back pain, I highly recommend the book Back Mechanic.
Schmorl’s Nodes: Genetic, or Environmental?
Although the immediate, mechanical causes of endplate damage are reasonably well understood, it wasn’t clear whether genetics played an important role in predisposing people to this type of injury. As the old saying goes, “Genetics loads the gun, and environment pulls the trigger.”
One study, published in 2007, set out to answer exactly this question.6
Study Design and Procedures
Researchers recruited 150 pairs of identical twins, and 366 pairs of fraternal twins from a UK twin registry. All of the subjects were adult women. On average, they were in their early 50s, measured about 162 cm (5 ft, 4 in) and weighed around 65 kg (143 lbs).
Twin pairs weren’t selected because of prior back pain, but they weren’t ruled out because of it either. During their evaluation, each twin completed a detailed questionnaire about their history of back pain.
45% of participants reported an episode of back pain that lasted for at least a month, while 19% reported some level of disability.
Each subject underwent an MRI scan, since MRIs are the preferred test for imaging disc material. Twin siblings were always scanned at the same appointment, and with the same machine.
These MRI images then underwent a simple evaluation. A doctor viewed the images of their T9–L5 spinal levels, and noted “0” (no Schmorl’s node) or “1” (Schmorl’s node present) at each.
Findings
The first noteworthy finding was that Schmorl’s nodes were pretty common. 30% of subjects had at least one node, and 14% had two or more.
They were more common in the thoracic region (59%) than the lumbar region (41%). The most common site of a Schmorl’s node was at T11.
This was in line with previous studies, which also showed that Schmoral’s nodes are more likely to occur in the thoracic region. One possible reason is that thoracic vertebrae are smaller than lumbar vertebrae, and therefore are less well-suited to handling stress.
Thoracic vertebrae are also able to twist more than lumbar vertebrae, and some researchers suspect that this twisting slowly damages the end plates.2
Some factors didn’t correlate with the presence of Schmorl’s nodes at all. These included BMI, smoking status, work history, and being pre- or post-menopausal.
There was an association between Schmorl’s nodes in the lumbar region, and lumbar disc degeneration. Although interestingly, there was no similar relationship between Schmorl’s nodes and disc degeneration at the thoracic level.
At first glance, it appeared that the presence of Schmorl’s nodes was associated with back pain. However, once researchers controlled for the association between Schmorl’s nodes and disc degeneration, this association became less striking.
The most notable conclusion, though, was the influence of genetics. In the thoracic region, the heritability estimate was a whopping 72%. In the lumbar region, it was even higher – 80%.
Conclusions
Endplate damage and Schmorl’s nodes are often due to compressive damage, which can occur gradually, or all at once. Some scientists believe that physical activity in adolescents, especially when it involves twisting, can also lead to endplate damage.
However, genetics is highly important in determining whether an individual will actually end up with a Schmorl’s node. The heritability estimate was 72% in the lumbar region, and 80% in the thoracic region.
In this case, genetics seems to load all the chambers in the gun.
References
- Adams, M A, and P Dolan. 1995. “Recent advances in lumbar spinal mechanics and their clinical significance.” Clinical Biomechanics (Elsevier Science Ltd) 10 (1): 3–19. doi:10.1016/0268-0033(95)90432-9.
- Dar, Gali, Youssef Masharawi, Smadar Peleg, Nili Steinberg, Hila May, Bahaa Medlej, Natan Peled, and Israel Hershkovitz. 2009. “Schmorl’s nodes distribution in the human spine and its possible etiology.” European Spine Journal (Springer) 19: 670–675. doi:10.1007/s00586-009-1238-8.
- Mattei, Tobias A, and Azeem A Rehman. 2013. “Schmorl’s nodes: current pathophysiological, diagnostic, and therapeutic paradigms.” Neurosurgical Review (Springer) 37: 39–46. doi:10.1007/s10143-013-0488-4.
- McGill, Stuart. 2016. Low Back Disorders: Evidence-Based Prevention and Rehabilitation. Third Edition. Human Kinetics.
- McGill, Stuart M. 1997. “The Biomechanics of Low Back Injury: Implications on Current Practice in Industry and the Clinic.” Journal of Biomechanics (Elsevier) 30 (5): 465–475. doi:10.1016/S0021-9290(96)00172-8.
- Williams, F MK, N J Manek, P N Sambrook, T D Spector, and A J MacGregor. 2007. “Schmorl’s Nodes: Common, Highly Heritable, and Related to Lumbar Disc Disease.” Arthritis & Rheumatism (American College of Rheumatology) 57 (5): 855–860. doi:10.1002/art.22789.
